Body Sites for Temperature Assessment
Body Sites for Temperature Assessment
An Overview of Temperature Measuring Sites
Oral Temperature
Oral temperature measurement is by far the most common clinical method in use today, and
is responsible for masking the greatest number of fevers. Oral temperature can be mislead-
ingly lowered by patient activity such as tachypnea, coughing, moaning, drinking, eating,
mouthbreathing, snoring, talking, etc. Alarmingly, another cause of low oral temperatures is
the fever itself. For each 0.6°C (1°F) temperature elevation, the pulse rate usually increases
approximately 10 beats per minute, there is a 7% increase in oxygen consumption, increas-
ing the respiratory rate approximately 2 cycles per
minute. The resulting increase in respiration can further
lower oral temperature sufficiently to mask a fever.
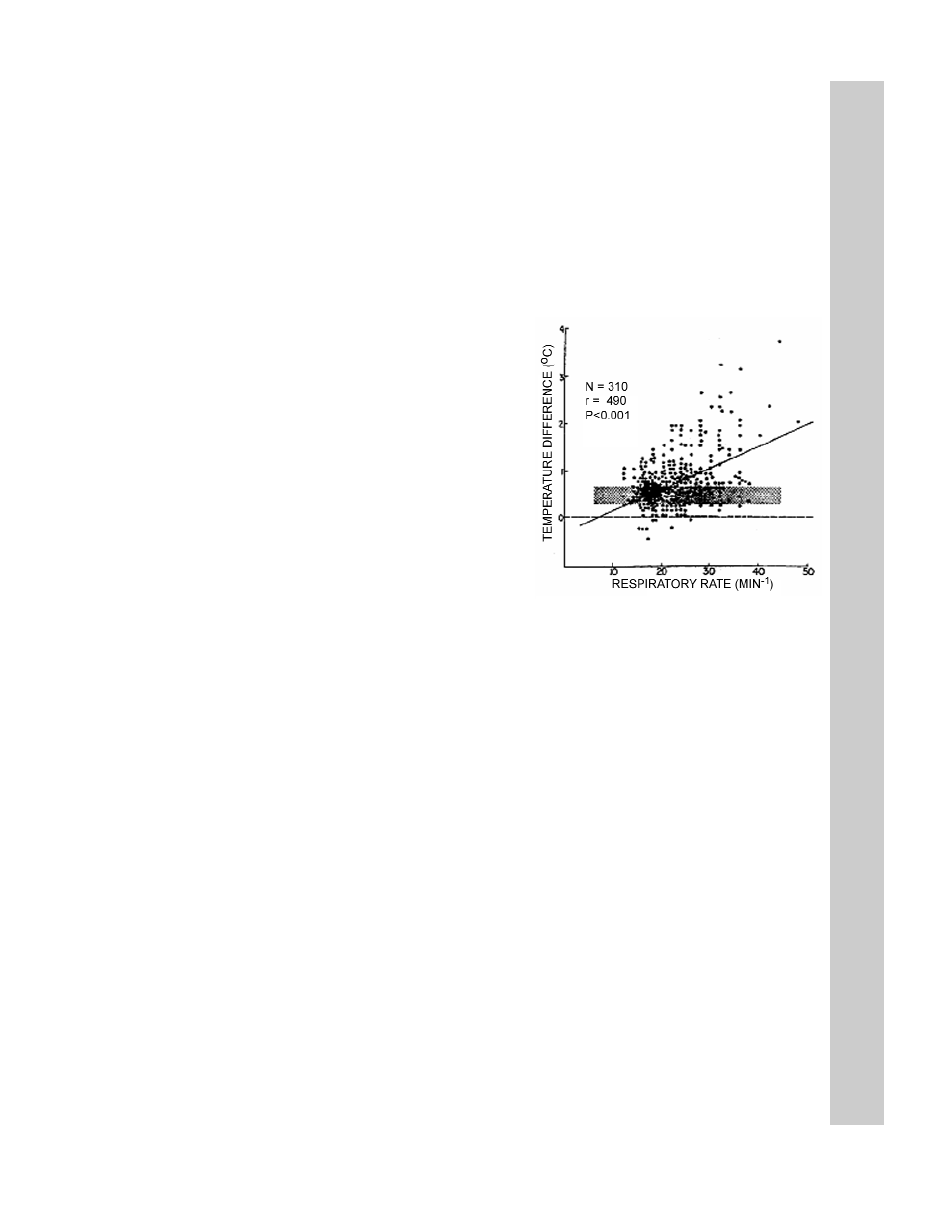
Figure 1 is of interest as it illustrates fever masking even
when clinicians had eliminated all obvious mouth-
breathers from the study. This emergency room study
presents the temperature difference (rectal minus oral) in
310 patients with a wide range of respiratory rates. The
straight line of best fit is shown. The stippled area
demonstrates the traditional normal difference between
rectal and oral temperature (0.3°- 0.65°C). The investi-
gators concluded that many patients with tachypnea
would have oral temperatures in the normal range
despite the presence of clinical fever, seriously mislead-
ing the clinician.
Rectal Temperature
Generally, rectal temperature is considered an indicator of
deep tissue and critical tissue temperatures, but long standing data demonstrate that rectal
temperature can be a lagging and unsatisfactory index. Fifty years ago, Eichna et al reported
differences between intracardiac, intravascular and rectal temperatures on afebrile patients to
be so insignificant that for all practical purposes, the temperatures may be considered to be the
same. Certainly rectal temperature is far less invasive than a pulmonary artery catheter, how-
ever, in the same study, data on febrile patients support sizeable differences.
Other comparisons between rectal, esophageal and aortic temperatures undertaken on
hypothermic patients by different researchers also confirm similar differences. Subsequent
but equally comprehensive comparisons on healthy volunteers further confirmed not only
temperature differences, but also quantified significant lags in rectal temperature vs. hypo-
thalamic temperature by times of order one hour. This is of interest since the blood as it
enters and affects the critical tissue in the hypothalamus should have considerable signifi-
cance in thermal homeostasis. However, this early data on hypothalamic temperature was
measured by a thermocouple inserted against (and often times perforating) the tympanic
membrane. With significant improvements in the methodology, more recent clinical observa-
tions show that the time constant of rectal temperature in critically ill patients may be consid-
erably longer, and in some cases, as much as a day.
Figure 1 Temperature Difference (Rectal
minus Oral) in 310 Patients with a Wide
Range of Respiratory Rates. The straight
line of best fit is shown. The stippled area
demonstrates the traditional “normal” differ-
ence between rectal and oral temperature
(0.3 to 0.65°C).
17
818528r5:818528r5.qxd 4/24/2008 11:04 AM Page 19


















